Call Us: (239) 221-6120
We are NOT currently hiring. This site is for families seeking memory care services. For employment inquiries, visit our Indeed page.
Redefining Memory Care In Estero Florida
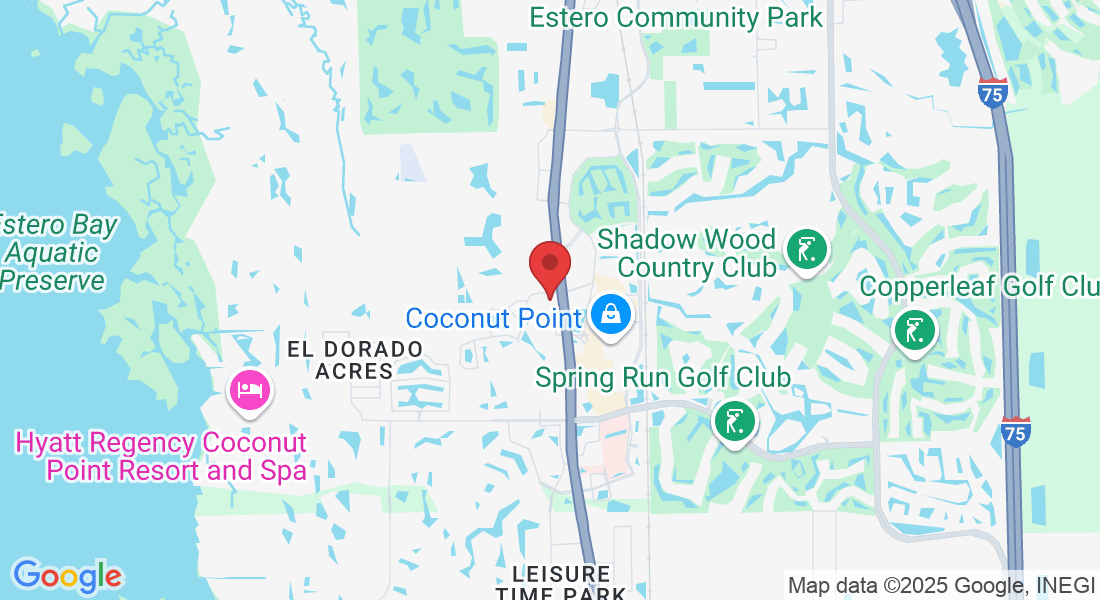
Choosing the right memory care community for a loved one is a deeply personal decision. At Gulf Coast Memory Care, conveniently located next to Coconut Point Shopping Center in Estero, Florida, we've created a haven of tranquility where residents can experience a luxurious and comfortable lifestyle. Let us help you make this important decision with confidence.
"Choose us with peace of mind; if within 90 days your heart pulls you elsewhere, we'll ensure a smooth transition and give your community fee back to help secure another place."
Your family's freedom to thrive is our top priority.

Award Winning Leadership

Understanding The Benefits Of Memory Care
Hear From Jen
We believe that exceptional care begins with open, honest, and ongoing communication. Families have direct access to our leadership and caregivers, including personal cell numbers, because staying informed should never be a struggle.
Every resident also receives a personalized care plan tailored to their needs, so families always stay connected.
Is It The Right Time For Memory Care?
Understanding that memory care is not a one-size-fits-all solution, we prioritize personalized care plans that adapt to each individual’s progression.
Learn more about senior care and get personalized results in this quick 5 minute survey.


A Community For Alzheimer’s & Dementia Care
Families seeking Alzheimer’s and dementia support in Estero, Florida, can rely on our compassionate team for a community that truly cares.
Through ongoing training in the latest memory care practices and a commitment to safety, Gulf Coast Memory Care offers peace of mind for families and the highest standard of care for residents.
Love From Our Families

My mom moved into her new home a few weeks ago. I was able to visit with her this week while being in Florida and my gosh, I know she is right where she needs to be. Huge shoutout to Jerry, Diana, Paula, Kathy and Apryl. You are real life angels. The energy you bring is above and beyond. To see how you interact with not only my mom, but all the residents, it truly warms my heart. While it is heartbreaking to see my mom battle Alzheimer's, I know she is in the perfect place. She is safe and receiving the care she needs. <3 The place is clean, accommodating and most importantly feels like home. I love that there is a schedule and many activities for the residents to participate in. My mom has loved the painting and coloring
- Bill & Bonny B

Shelly Richardson

Upon entering this beautiful community, I was deeply impressed by the exceptional level of care and compassion demonstrated by all the caregivers. Every member of the team, from maintenance staff to the executive director, significantly contributes to the residents' quality of life. The interior courtyards offer a safe and beautiful outdoor escape for the residents, while the dining area is both elegant and spacious. GCMC stands out as one of the premier memory care centers I have ever visited.
- Bill & Bonny B


Exceptional dedication. Genuine care 24/7, everyone is doing a great job, from Management to the care team. Jerry and Diana are conducting the business, but you can see them walking the hallway and chatting with the residents, literally knowing everyone. There is an engine who works behind the scenes to have the day and night activity running smoothly. Family feeling, warmth, and genuine care, overall, 5 stars. Residents are never alone, there is always a pair of eyes to watch and hands ready to help as needed, but all is done in a certain way, so our loved ones don’t feel any loss of their independence. Beautifully done. The activities are not just lines on paper, everyone is involved. Food is first class.
- Bill & Bonny B
Our Senior Care Amenities

One-site beauty salon and barbershop
Personalized, chef-prepared meals
Customized activity programs
Craft and hobby room
Family living room
Full Library
Abundant natural light to minimize sundowning
Located next to Coconut Point Shopping Center
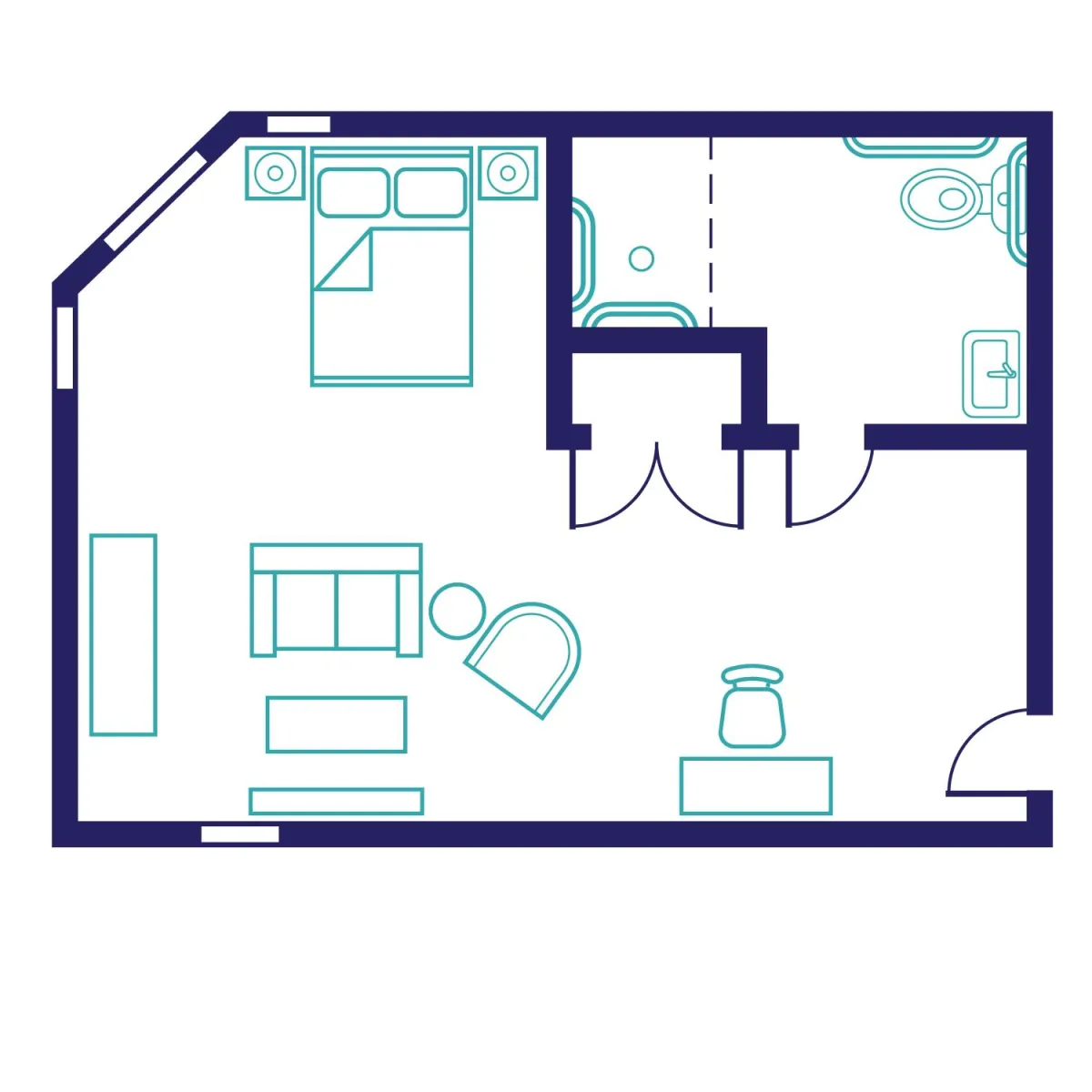
The Edison Suite

The Magnolia Suite
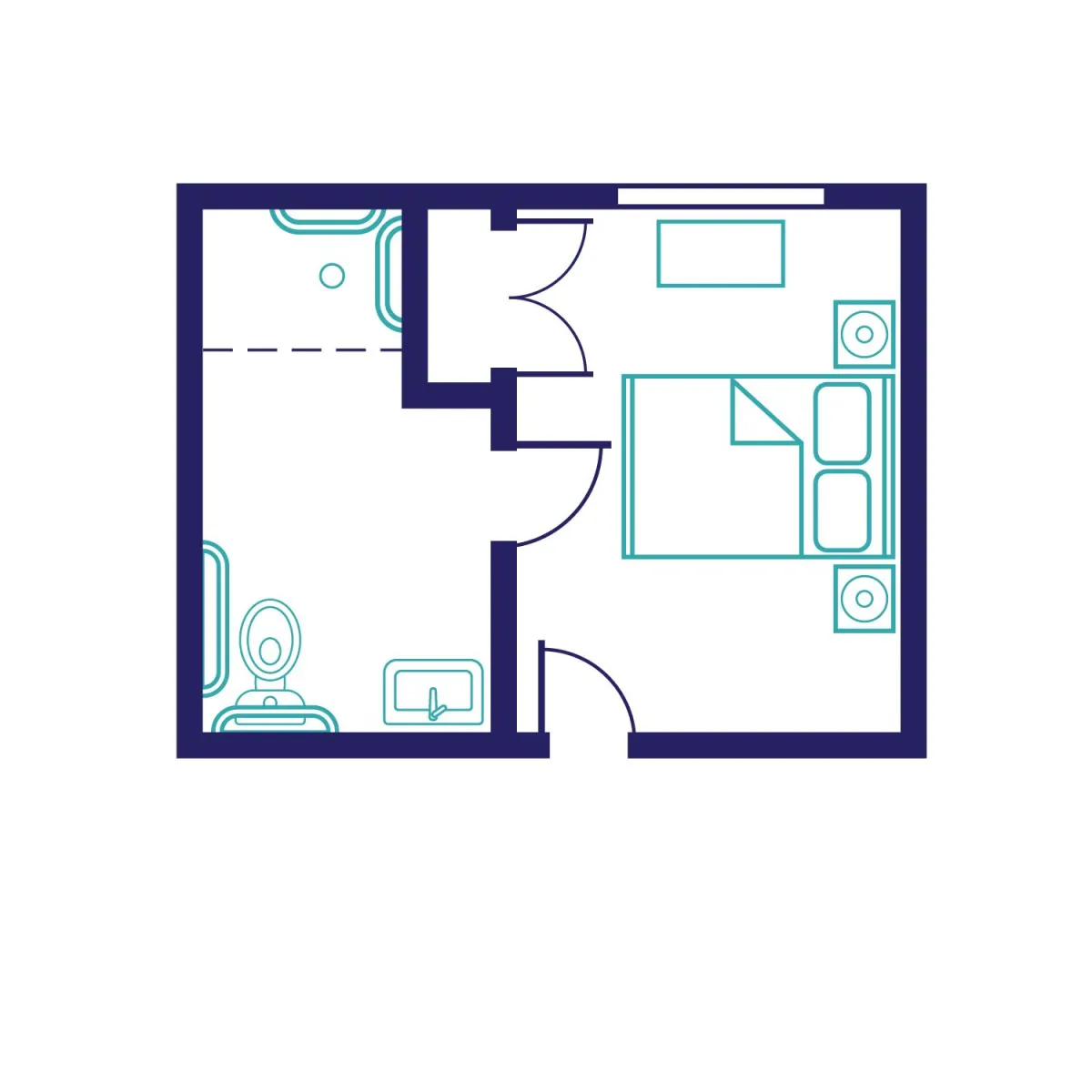
The Sugarberry Suite

Engaging Residents With Meaningful Social Connections
We also prioritize activities that nurture both physical and mental wellness, from gentle exercise routines to social events that create a sense of community among residents. These carefully crafted programs are designed to boost mood, reduce anxiety, and encourage meaningful interactions, all of which contribute to a fulfilling lifestyle for those facing memory challenges.
Our Commitment To You
Our commitment extends to providing families with guidance and resources to understand memory loss and navigate the journey with confidence. Whether it’s through educational workshops or one-on-one consultations, we’re here to support families every step of the way, ensuring they feel connected and informed about their loved one’s care journey.


Are You Ready To Get Settled In?
Embark on a transformative experience at Gulf Coast Memory Care in Estero, Florida. We're not just a memory care community; we're a sanctuary where the mind, body, and spirit are nurtured. If you're seeking a place where compassion, care, and a deep respect for the human soul are paramount, you've found the right haven.
Check Out Our Blog

When They Ask 'When Can I Go Home?': Compassionate Responses for Memory Care Families
One of the most heartbreaking moments families face in memory care is hearing their loved one ask, "When can I go home?" This question—repeated daily, sometimes hourly—leaves families feeling guilty, helpless, and emotionally devastated. At Gulf Coast Memory Care, we understand this universal experience and want to help you respond with compassion and confidence.
Understanding Why They Ask to Go Home
The Question Behind the Question
When residents ask to go home, they're rarely asking about a physical location. Instead, they're expressing:
A need for comfort and security
Feelings of confusion or anxiety
A desire to return to a familiar time in their life
Emotional distress they can't articulate differently
How Dementia Changes Perception
Dementia affects the brain's ability to:
Process current location and time
Recognize familiar environments
Distinguish between past and present
Feel secure in new surroundings
What NOT to Say (And Why)
Avoid These Common Responses
"You ARE home." Why it doesn't work: This can increase confusion and agitation when the environment doesn't match their memory of "home."
"Don't you remember? We talked about this." Why it doesn't work: Highlighting memory loss increases frustration and embarrassment.
"You can't go home because [reason]." Why it doesn't work: Logic doesn't work with dementia. Rational explanations often increase distress.
"Stop asking that question." Why it doesn't work: Dismissing their feelings damages trust and increases anxiety.
Compassionate Response Strategies
The Validation Approach
What to say: "Tell me about your home. What do you miss most?"
Why it works:
Validates their feelings
Redirects to positive memories
Creates connection through conversation
Reduces immediate anxiety
The Comfort Response
What to say: "I can see you're feeling uncomfortable. Let's find something that helps you feel better."
Why it works:
Acknowledges their emotional state
Offers immediate support
Focuses on present comfort
Avoids confrontation about location
The Redirection Technique
What to say: "That sounds nice. Would you like to [activity] while we talk about it?"
Why it works:
Doesn't dismiss their request
Introduces calming activity
Shifts focus gently
Maintains dignity
The Time-Based Response
What to say: "We'll talk about that after [meal/activity]. Right now, let's [immediate activity]."
Why it works:
Provides a "later" without promising specifics
Offers immediate alternative
Reduces urgency of the request
GCMC's Staff Training in Communication
Teepa Snow Methods
Our caregivers receive specialized training in:
Recognizing emotional needs behind questions
Using body language to convey safety
De-escalation techniques
Validation therapy approaches
Creating moments of connection
24/7 Specialized Support
With our 8:1 staff-to-resident ratio, team members can:
Respond immediately to distress
Spend quality time understanding individual triggers
Provide personalized comfort strategies
Maintain consistency in communication approaches
Creating "Home" Feelings in Memory Care
Environmental Comfort
At GCMC, we create home-like feelings through:
Abundant natural light
Comfortable, familiar furnishings
Personal suite customization
Interior courtyards for outdoor comfort
Routine and Familiarity
Our Rhythm of Life programming provides:
Consistent daily schedules
Familiar activities
Predictable meal times
Comforting rituals
Personal Connections
We foster "home" feelings by:
Learning residents' life histories
Incorporating personal preferences
Celebrating individual traditions
Building genuine relationships
Supporting Families Through This Challenge
Managing Your Own Emotions
It's Normal to Feel:
Heartbreak hearing the question repeatedly
Frustration at not being able to "fix" it
Grief for the relationship changes
Remember:
You made the best decision for their safety
Professional care provides what home cannot
Your love hasn't changed
This is the disease speaking, not rejection of you
Visit Strategies
Before Visits:
Prepare emotionally for the question
Have redirection strategies ready
Bring comfort items or photos
During Visits:
Focus on present moment activities
Engage in familiar, enjoyable activities
Stay calm if the question arises
Use validation and redirection techniques
After Visits:
Process your emotions with support
Remember the positive moments
Trust the professional care team
Practice self-compassion
When to Seek Additional Support
Signs Your Loved One Needs Extra Help
Increased agitation around "going home"
Physical attempts to leave
Distress lasting beyond brief episodes
Changes in sleep or eating patterns
GCMC's Response
Our team:
Monitors behavioral patterns
Adjusts care plans as needed
Communicates changes with families
Collaborates with medical partners when necessary
Frequently Asked Questions
Q: Will they ever stop asking to go home? A: The frequency often decreases as residents become more comfortable and familiar with their environment. Some residents continue asking but with less distress.
Q: Should I visit less if they always ask to go home when I leave? A: Not necessarily. Work with staff to find the right visit frequency and duration. Sometimes shorter, more frequent visits work better.
Q: Is it okay to lie about why they can't go home? A: We prefer "therapeutic fibbing" or redirection over direct lies. Focus on emotional truth rather than factual details.
Q: How do I explain this to other family members who don't understand? A: Share educational resources about dementia communication. Invite them to speak with our staff about why certain responses work better.
The Power of Trained Communication
Real-World Impact
When staff understand dementia communication:
Residents experience less agitation
Families feel more supported
Trust builds between residents and caregivers
Quality of life improves significantly
GCMC's Commitment
Every team member receives ongoing training in:
Compassionate communication
Behavior management
De-escalation techniques
Understanding the emotional world of dementia
Key Takeaways
✓ "When can I go home?" expresses emotional needs, not literal requests
✓ Validation works better than logic or correction
✓ Redirection and comfort reduce distress
✓ Professional training makes a significant difference
✓ You're not alone in facing this challenge
✓ Creating "home" feelings is possible in memory care
Moving Forward with Compassion
Hearing your loved one ask to go home never gets easier, but understanding the question behind the question helps you respond with compassion rather than guilt. At Gulf Coast Memory Care, our staff's specialized training in Teepa Snow methods and dementia communication ensures your loved one receives responses that comfort rather than confuse.
You don't have to navigate this alone. Our team is here to support both residents and families through every challenging moment, providing guidance, understanding, and professional expertise.
Struggling with communication challenges in memory care? Contact Gulf Coast Memory Care to learn how our specialized training and compassionate approach support families through difficult moments. Schedule a tour to see our communication strategies in action.

When They Ask 'When Can I Go Home?': Compassionate Responses for Memory Care Families
One of the most heartbreaking moments families face in memory care is hearing their loved one ask, "When can I go home?" This question—repeated daily, sometimes hourly—leaves families feeling guilty, helpless, and emotionally devastated. At Gulf Coast Memory Care, we understand this universal experience and want to help you respond with compassion and confidence.
Understanding Why They Ask to Go Home
The Question Behind the Question
When residents ask to go home, they're rarely asking about a physical location. Instead, they're expressing:
A need for comfort and security
Feelings of confusion or anxiety
A desire to return to a familiar time in their life
Emotional distress they can't articulate differently
How Dementia Changes Perception
Dementia affects the brain's ability to:
Process current location and time
Recognize familiar environments
Distinguish between past and present
Feel secure in new surroundings
What NOT to Say (And Why)
Avoid These Common Responses
"You ARE home." Why it doesn't work: This can increase confusion and agitation when the environment doesn't match their memory of "home."
"Don't you remember? We talked about this." Why it doesn't work: Highlighting memory loss increases frustration and embarrassment.
"You can't go home because [reason]." Why it doesn't work: Logic doesn't work with dementia. Rational explanations often increase distress.
"Stop asking that question." Why it doesn't work: Dismissing their feelings damages trust and increases anxiety.
Compassionate Response Strategies
The Validation Approach
What to say: "Tell me about your home. What do you miss most?"
Why it works:
Validates their feelings
Redirects to positive memories
Creates connection through conversation
Reduces immediate anxiety
The Comfort Response
What to say: "I can see you're feeling uncomfortable. Let's find something that helps you feel better."
Why it works:
Acknowledges their emotional state
Offers immediate support
Focuses on present comfort
Avoids confrontation about location
The Redirection Technique
What to say: "That sounds nice. Would you like to [activity] while we talk about it?"
Why it works:
Doesn't dismiss their request
Introduces calming activity
Shifts focus gently
Maintains dignity
The Time-Based Response
What to say: "We'll talk about that after [meal/activity]. Right now, let's [immediate activity]."
Why it works:
Provides a "later" without promising specifics
Offers immediate alternative
Reduces urgency of the request
GCMC's Staff Training in Communication
Teepa Snow Methods
Our caregivers receive specialized training in:
Recognizing emotional needs behind questions
Using body language to convey safety
De-escalation techniques
Validation therapy approaches
Creating moments of connection
24/7 Specialized Support
With our 8:1 staff-to-resident ratio, team members can:
Respond immediately to distress
Spend quality time understanding individual triggers
Provide personalized comfort strategies
Maintain consistency in communication approaches
Creating "Home" Feelings in Memory Care
Environmental Comfort
At GCMC, we create home-like feelings through:
Abundant natural light
Comfortable, familiar furnishings
Personal suite customization
Interior courtyards for outdoor comfort
Routine and Familiarity
Our Rhythm of Life programming provides:
Consistent daily schedules
Familiar activities
Predictable meal times
Comforting rituals
Personal Connections
We foster "home" feelings by:
Learning residents' life histories
Incorporating personal preferences
Celebrating individual traditions
Building genuine relationships
Supporting Families Through This Challenge
Managing Your Own Emotions
It's Normal to Feel:
Heartbreak hearing the question repeatedly
Frustration at not being able to "fix" it
Grief for the relationship changes
Remember:
You made the best decision for their safety
Professional care provides what home cannot
Your love hasn't changed
This is the disease speaking, not rejection of you
Visit Strategies
Before Visits:
Prepare emotionally for the question
Have redirection strategies ready
Bring comfort items or photos
During Visits:
Focus on present moment activities
Engage in familiar, enjoyable activities
Stay calm if the question arises
Use validation and redirection techniques
After Visits:
Process your emotions with support
Remember the positive moments
Trust the professional care team
Practice self-compassion
When to Seek Additional Support
Signs Your Loved One Needs Extra Help
Increased agitation around "going home"
Physical attempts to leave
Distress lasting beyond brief episodes
Changes in sleep or eating patterns
GCMC's Response
Our team:
Monitors behavioral patterns
Adjusts care plans as needed
Communicates changes with families
Collaborates with medical partners when necessary
Frequently Asked Questions
Q: Will they ever stop asking to go home? A: The frequency often decreases as residents become more comfortable and familiar with their environment. Some residents continue asking but with less distress.
Q: Should I visit less if they always ask to go home when I leave? A: Not necessarily. Work with staff to find the right visit frequency and duration. Sometimes shorter, more frequent visits work better.
Q: Is it okay to lie about why they can't go home? A: We prefer "therapeutic fibbing" or redirection over direct lies. Focus on emotional truth rather than factual details.
Q: How do I explain this to other family members who don't understand? A: Share educational resources about dementia communication. Invite them to speak with our staff about why certain responses work better.
The Power of Trained Communication
Real-World Impact
When staff understand dementia communication:
Residents experience less agitation
Families feel more supported
Trust builds between residents and caregivers
Quality of life improves significantly
GCMC's Commitment
Every team member receives ongoing training in:
Compassionate communication
Behavior management
De-escalation techniques
Understanding the emotional world of dementia
Key Takeaways
✓ "When can I go home?" expresses emotional needs, not literal requests
✓ Validation works better than logic or correction
✓ Redirection and comfort reduce distress
✓ Professional training makes a significant difference
✓ You're not alone in facing this challenge
✓ Creating "home" feelings is possible in memory care
Moving Forward with Compassion
Hearing your loved one ask to go home never gets easier, but understanding the question behind the question helps you respond with compassion rather than guilt. At Gulf Coast Memory Care, our staff's specialized training in Teepa Snow methods and dementia communication ensures your loved one receives responses that comfort rather than confuse.
You don't have to navigate this alone. Our team is here to support both residents and families through every challenging moment, providing guidance, understanding, and professional expertise.
Struggling with communication challenges in memory care? Contact Gulf Coast Memory Care to learn how our specialized training and compassionate approach support families through difficult moments. Schedule a tour to see our communication strategies in action.
Come Visit Us
We can't wait to hear from you! Fill out our contact form to get started or if you would like to see our community for yourself, schedule a tour here.
Gulf Coast Memory Care
(239) 221-6120
22900 Lyden Dr, Estero, FL 33928
AL# 12921
Privacy Policy | Accessibility Statement | Visitation Policy